Saturday, October 24, 2009
Eyes, Eye disease , Pupil
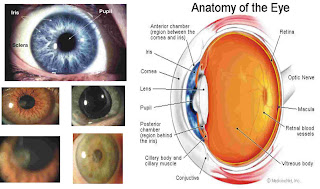
Eyes
Eyes are organs of vision that detect light to distinguish color and read, which is the simplest eyes nothing else but to know whether the surroundings are light or dark.the part of the eye
The cornea is the outermost part of the eyeball that receives light from light sources.
Pupil and Iris from the cornea, the light will be forwarded to the pupils. Pupils determine the quantity of light entering the greater part of the eye. Pupils will be widened if the dark room conditions, and will be narrowed if the room light conditions. Wide pupils affected by the slice in sekelilingnya.Iris serves as the diaphragm. Iris is seen as part of the color on the eyes.
Lens of the eye receives light from the pupil and pass them on to the retina. The function is the eye lens focus the light, so that the light falls exactly on the retina of yellow spots. To see a distant object (the light coming from far away), eye lens will be thinner. As for seeing near objects (the light comes from the close), will thicken the eye lens.
Retina of the eye is most sensitive to light, particularly the retina called the yellow dots. After the retina, the light transmitted to the optic nerve.
Neural cells into the ropes and cones in the retina, to go to the brain.
Eye disease
Myopia ie someone who can not see distant objects. Usually occurs in students.
Hipermetropi is a user who can not see distant objects near the eye.
Presbiopi is someone who can not see distant objects near or far away. Common in the elderly.
Myopia and blindness, blind means a person can not see any thing at all. Blind could have caused the descendants, as well as accidents. Blindness means that a person can only see dimly. The people who are blind or myopic usually "read" with her fingers. This is called Braille.
Color blindness is a condition where a person is not able to distinguish colors. Which can be seen only in black, gray, and white. Color blindness is usually hereditary. This means that if someone is color blind, almost certainly his son is also color blind.
Cataract is an eye disease in which the lens of the eye becomes opaque and occurs in the elderly (seniors).
Stomach
Stomach or ventrikulus form a pouch located under the diaphragm. Stomach can be divided into three regions, namely the cardia, fundus and pylorus. Cardia is the top, the entrance area of food from the esophagus. Fundus is the middle, rounded shape. Pylorus is the lower part, the area associated with the 12 finger intestine (duodenum). On the wall of the inner hull are the glands that produce gastric lymph. The smell, shape, color and taste of food will cause reflex secretion of gastric lymph. Sap stomach gastric acid (HCl), pepsin, musin, and renin. Gastric acid serves as a killer of microorganisms and activates the enzyme pepsinogen into pepsin. Pepsin is an enzyme that can change the protein into smaller molecules. Musin is smoothed mucosal protein foods. Renin is a specific enzyme found only in mammals, acting as kaseinogen into casein. Casein coagulated by Ca ² + from milk that can be digested by pepsin. Without a tangible case reninm liquid will slip in and USU lambuing without a chance to digest.
Duodenum, Pars superior, pars descendens, Pars horizontalis
Duodenum
Duodenum or duodenum is a part of the small intestine that is located after the stomach and connecting it to the empty intestine (jejunum). Bowel twelve finger is the shortest part of the small intestine, starting from the bulbo duodenale and ends at Treitz ligament. Duodenum is a retroperitoneal organ, which is not covered entirely by the peritoneal membrane. intestinal pH twelve fingers normal range in nine degrees.Duodenum is responsible for distributing food to the small intestine. Histologically, there Brunner glands that produce mucus. Twelve of the intestinal wall is composed of fingers layers of very thin cells that form the mucosal muscles.
Parts Duodenum, Pars superior first part, which starts from suoerior Pars end of the pylorus pylorus is the lower part, the area associated with the 12 finger intestine (duodenum). Then the channel will be pulled into the right lateral. This section has a length of 5 cm. The second part of pars descendens, descendens pars continue the first part. This section bebentuk straight down the channel, In this section there is the estuary of the pancreatic duct and bile duct communis which coalesce into hepatopankreatika duct. In addition, a bulge terdpaat also called duodeni papilla.Pars horizontalis third section, Pars horizontalis shaped horizontal channel, through the inferior vena cava, aorta, and spine. Pars ascendens last section, funnel-shaped pars ascendens ascending and ends at the beginning of the empty intestine (jejunum).
Brunner's glands are submucosal glands in the duodenum. Its main function is to produce alkaline secretion containing bicarbonate for :
- Protect the duodenum from acid substances from the judge (a collection of food from the previous digestion).
- as a lubricant of the intestinal wall.
- provide alkaline conditions for intestinal enzymes to be active. The enzyme functions to start the absorption.Enzymes are biomolecules that serve as a catalyst (substance that speeds up the reaction without reacting) in a chemical reaction, the enzyme works by attaching molecules to the surface of substances that react and thus accelerate the reaction process, enzyme Work influenced by several factors, especially is the substrate, temperature, acidity, cofactors and inhibitors. Each enzyme requires the temperature and pH (acidity level) optimum different because enzymes are proteins, which can change shape if the temperature and acidity changes.
Labels:
Duodenum,
pars descendens,
Pars horizontalis,
Pars superior
Friday, October 16, 2009
The Formation Process of Male Fetuses and Female

The process of formation of male fetuses and female gonads begins from the formation. Initially sperm cells have a Y chromosome will be formed into the male organ and the organ of the female X. Further differentiation to form testes Y chromosome X chromosome while forming the ovary. The process of formation of the testes started from the degeneration of the gonad cortex and medulla semineferus gonadal tubules form. In the gap mesenchyme cells formed tubular networks along intertistial Leydig cells. Leydig cells with Sertoli cells to form testosterone and duct muller muller but duct degeneration due to form factor muller anti ducts, testosterone is formed into the epididymis, vas deferent, vesicles and ducts seminlis mesonephros. Because there are enzymes to form 5 alfareduktase differentiation testosterone to dihydrotestosterone which is formed on the epithelium of the urethra and prostate bulbouretra, experienced swelling and formed scrotum. Then the testes descended into the pelvis all the way to the scrotum. First notch testes in the scrotum scrotum will increasingly separate from the testis of the pelvic cavity.
While the X chromosome which has undergone further differentiation and degenerate primers form a pit filled medullary mesenchyme and blood vessels, forming thickened germinal epithelium of the developing follicle cells into the egg follicles. So ovarian gonadal differentiation occurs after a few days defrensiasi testis. Here fostering growth of ovarian cortex while the medulla shrunk. PGH placenta growth of stem cells into oogonia, and then formed into plorifrasi primary oocyte. In women mesonephros duct degeneration. As the forming gonadal differentiation into ovaries down to the pelvic cavity and then whirled around 450 cross-located.
Penis and the clitoris at the initial growth of invagina ectoderm. The clitoris is actually a penis that is not completely developed. The males grow with evagina ectoderm carried sinus urogenitalis from cloaca.
Penis and the clitoris at the initial growth of invagina ectoderm. The clitoris is actually a penis that is not completely developed. The males grow with evagina ectoderm carried sinus urogenitalis from cloaca.
Baby Expenses
Birth divided into several stages. The first stage, the process of childbirth. In this stage there opening (dilating) the mouth of the womb until full. Furthermore, the second stage is the birth of the baby out safely. The third stage, the placenta expenses. The next stage is the observation of the mother for an hour after the placenta came out.
The first stage is a contraction. This is usually the longest phase. The opening of the cervix (dilation) to 3 cm, was also accompanied by depletion (effasi). This could happen within a few days, even weeks, without contraction means (less than one minute). But in some people may have happened only 2-6 hours (or even all 24 hours) with a contraction more clearly. After the cervix is more lebar.Umumnya this phase is shorter than the previous phase, lasts about 2-3 hours. Strong contractions occur about 1 minute, more regular pattern with a distance of 4-5 minutes. The cervix opens to 7 cm.
In general, normal, dilation of the cervix will continue to increase with stronger contractions. Occurs once during the 2-3 minutes 1.5 minutes with peak contraction so strong that she felt as if contraction occurs continuously without any pause.
The first stage is a contraction. This is usually the longest phase. The opening of the cervix (dilation) to 3 cm, was also accompanied by depletion (effasi). This could happen within a few days, even weeks, without contraction means (less than one minute). But in some people may have happened only 2-6 hours (or even all 24 hours) with more jelas.fase contraction was shorter than the previous phase, lasts about 2-3 hours. Strong contractions occur about 1 minute, more regular pattern with a distance of 4-5 minutes. The cervix opens to 7 cm.
In general, normal, dilation of the cervix will continue to increase with stronger contractions. Occurs once during the 2-3 minutes 1.5 minutes with peak contraction so strong that she felt as if contraction occurs continuously without any pause.
The opening of the cervix from 3 cm to 10 cm occurred very short, about 15 minutes to 1 hour. Currently prospective mother will feel very strong pressure on the lower back. Similarly, the pressure on the anus with the urge to push. Mother would feel hot and cold sweats.
The position of expectant mothers in childbirth helped smooth delivery. Half-sitting position or half-squat position may be best for this position using gravity, thrust and increase capital.
Expenditures placenta
Maternal exhaustion is left when the baby is out, but the task has not ended. Placenta that had been supporting the baby to life in the womb must be removed.
uterine cavity has narrowed so as to separate the placenta from the uterine wall and moving it down to the bottom of the uterus or the vagina. Mom just pushed as pushing the baby out. It's just not the energy released as powerful as the baby's expenses. If the placenta is out, will soon tear or episiotomy stitches so right again.
While the X chromosome which has undergone further differentiation and degenerate primers form a pit filled medullary mesenchyme and blood vessels, forming thickened germinal epithelium of the developing follicle cells into the egg follicles. So ovarian gonadal differentiation occurs after a few days defrensiasi testis. Here fostering growth of ovarian cortex while the medulla shrunk. PGH placenta growth of stem cells into oogonia, and then formed into plorifrasi primary oocyte. In women mesonephros duct degeneration. As the forming gonadal differentiation into ovaries down to the pelvic cavity and then whirled around 450 cross-located.
Penis and the clitoris at the initial growth of invagina ectoderm. The clitoris is actually a penis that is not completely developed. The males grow with evagina ectoderm carried sinus urogenitalis from cloaca.
Penis and the clitoris at the initial growth of invagina ectoderm. The clitoris is actually a penis that is not completely developed. The males grow with evagina ectoderm carried sinus urogenitalis from cloaca.
Baby Expenses
Birth divided into several stages. The first stage, the process of childbirth. In this stage there opening (dilating) the mouth of the womb until full. Furthermore, the second stage is the birth of the baby out safely. The third stage, the placenta expenses. The next stage is the observation of the mother for an hour after the placenta came out.
The first stage is a contraction. This is usually the longest phase. The opening of the cervix (dilation) to 3 cm, was also accompanied by depletion (effasi). This could happen within a few days, even weeks, without contraction means (less than one minute). But in some people may have happened only 2-6 hours (or even all 24 hours) with a contraction more clearly. After the cervix is more lebar.Umumnya this phase is shorter than the previous phase, lasts about 2-3 hours. Strong contractions occur about 1 minute, more regular pattern with a distance of 4-5 minutes. The cervix opens to 7 cm.
In general, normal, dilation of the cervix will continue to increase with stronger contractions. Occurs once during the 2-3 minutes 1.5 minutes with peak contraction so strong that she felt as if contraction occurs continuously without any pause.
The first stage is a contraction. This is usually the longest phase. The opening of the cervix (dilation) to 3 cm, was also accompanied by depletion (effasi). This could happen within a few days, even weeks, without contraction means (less than one minute). But in some people may have happened only 2-6 hours (or even all 24 hours) with more jelas.fase contraction was shorter than the previous phase, lasts about 2-3 hours. Strong contractions occur about 1 minute, more regular pattern with a distance of 4-5 minutes. The cervix opens to 7 cm.
In general, normal, dilation of the cervix will continue to increase with stronger contractions. Occurs once during the 2-3 minutes 1.5 minutes with peak contraction so strong that she felt as if contraction occurs continuously without any pause.
The opening of the cervix from 3 cm to 10 cm occurred very short, about 15 minutes to 1 hour. Currently prospective mother will feel very strong pressure on the lower back. Similarly, the pressure on the anus with the urge to push. Mother would feel hot and cold sweats.
The position of expectant mothers in childbirth helped smooth delivery. Half-sitting position or half-squat position may be best for this position using gravity, thrust and increase capital.
Expenditures placenta
Maternal exhaustion is left when the baby is out, but the task has not ended. Placenta that had been supporting the baby to life in the womb must be removed.
uterine cavity has narrowed so as to separate the placenta from the uterine wall and moving it down to the bottom of the uterus or the vagina. Mom just pushed as pushing the baby out. It's just not the energy released as powerful as the baby's expenses. If the placenta is out, will soon tear or episiotomy stitches so right again.
Fetal Development in the Uterus

Cleavage
According to the orphans (1990:155) on human holobastik cleavage occurs irregularly. Where the field and when the stages are not the same division and not simultaneously in various regions zygote. Initially the zygote divides into 2 cells, then place the cells 3 and 4 levels of the cell, continued levels of 5 cell, 6 cell, 7 cells, 8 cells, and continuously until balstomer formed consisting of 60-70 cells, a massive clump of called Morula.
Cleavage or segmentation occurs after cleavage. Zygote divides repeatedly to consist of scores of small cells called a blastomere. Cleavage that covers all parts of the bias, the bias is also only a small part of the zygote. This cleavage occurs in mitosis. Field direction taken by the cleavage of the zygote through continuous mitotic into many cells, called the field division. There are 4 kinds of cleavage of the meridian, vertical, and latitudinal equator.
Blastulasi and Nidasi
After Morula cells experiencing constant division will be formed cavity in the middle. This cavity increasingly large and filled with fluid. Embryo that has a cavity called a blastula, blastocoel called sockets, a process called blastulasi blastula formation.
Blastula formed division until this happens on the oviduct and lasted for 5 days. Next blastula will flow to the uterus. After entering the uterus, blastosis first floated in uteus lumen. Then, 6-7 days after fertilization embryos will hold the relationship with the wall of the uterus to develop into the next stage. Events relationship between embryo in the uterus called the endometrium of implantation or nidasi. This implantation is complete in 12 days after fertilization (Orphan, 1990: 136). Gastrulasi
According to Tenzer (2000:212) After the blastula stage is complete proceed to the gastrulation stage. Gastrula place on day 15. Gastrula stage is a stage or the most critical stage for the embryo. Gastrulation occurs at the dynamic development of embryos due to cell migration, changes in cell shape and organization of an embryo in the axis system. The original set of cells located far apart, it is located close enough to make stimulating interaction in the formation of a system organs. Gastrulation produces 3 layers of institutions in the next layer of endoderm, mesoderm and ectoderm adjacent to the middle on the outside.
In the process of gastrulation occurs in addition to continuous cell division and multiplication, there are various kinds of cell movements in the effort to regulate and develop in accordance with the shape and body composition of individuals of the species concerned.
Tubulasi
Tubulasi is the growth that accompanied formation of gastrula or collectively, the pembumbungan. The regions forming tool or going to the third seed layers ectoderm, mesoderm and endoderm, arrange themselves so that a tube, hollow. Pembumbungan who did not experience the notochord, but massive. Accompany the process tubulasi local differentiation process occurs in three layers of each tube of seeds, which in the next growth will develop instruments (organ) form definitive. When tubulasi neural ectoderm in progress, the early differentiation also occurred in areas that pipe, the front of the body becomes encephalon (brain) and the back of the spinal cord of the neural tube (neural). Endoderm tube occurs at the early differentiation of the front line, middle and rear. On the tube mesoderm occurs early differentiation of skeletal muscle to grow, the skin dermis and other connective tissue, muscle, viscera, the framework and tools urogenitalia.
Organogenesis
Organogenesis or embryo morphogenesis is a primitive form that evolved into a more definitive shape and appearance memmiliki specific within a species. Organogensisi the weekend begins and ends at the 3 end of the week to 8. With the end of the organogenesis external characteristic and major organ systems have formed, hereinafter called the fetus embryo (Amy Tenzer, et al, 2000)
In the period of growth or transition occurs between transformation and differentiation of parts, embryos from primitive forms to become the definitive form. In this period embryos will have a special form for a species. At the end of growth period, the smooth completion of definitive shape that is characteristic of an individual. In this period of embryo growth experienced resolution of gender, character (physical characteristics and psychological) and special face for each individual. Organogenesis in the tube-tube:
Tube epidermal
- Epidermal layer of skin, with a textured derivation (chemical composition) horn: scales, feathers, hooves, horns, horns, spurs.
- Skin glands: hair oil glands, sweat glands, salivary glands, glands lenders, tear glands.
- Lens of the eye, ear instruments, senses the smell and the sense of touch.
- Stomodeum grow up, with a derivation such as tooth enamel coating, salivary glands and the sense of taste.
- Proctodeum grow with rectal gland that produces odor.
- Tooth enamel.
- Epithelial layer of the entire digestive tract from the pharynx to the rectum.
- Digestive glands such as the liver, pancreas, and glands containing enzyme lenders in esophageal, gastric and intestium.
- Pulmonary epithelial layer or gill.
- Cloaca is the estuary of three channels: disposal (ureter), food (rectum), and venereal (genital ductus).
- Epithelial layer of the vagina, urethra, urinary and glandular vesika-gland.
- The brain and spinal cord.
- Peripheral nervous brain and spine.
- Part sensory nerves, such as eyes, nose and skin.
- Chromatophore skin and organs that have pigment.
- Muscle: striated, smooth and cardiac.
- Mesenchyme differentiation that can be a variety of cells and tissues
- Gonads, channels, and gland-gland.
- Kidney and ureter.
- Layers of muscle and connective tissue (Tunica muscularis, adventitia Tunica, Tunica musclarismucosa and serous) the various channels in the body, such as digestion, sex, trachea, bronchi, and blood vessels.
- Layers of the body cavity and membranes various tools: plera, pericardium, peritoneum and mesentery.
- Connective tissue in tools such as liver, pancreas, clogged gland.
- Layer of dentin, cementum and dental periodontum, with pulpanya.
Fetus Development Stage / Fetus
Stage of fetal development to begin in 3 to 10. In the last 6 months of human development is used to increase the size and mature organs formed in the first 3 months.
By the time the fetus entered the 3-month, 40 mm in length. Fetal organs already have such systems possessed by an adult. At this age can not be distinguished genital between males and females, and looks like a female and heart rate can already be heard.
In the last 6 months of human development is used to increase the size and mature organs formed in the first 3 months.
By the time the fetus entered the 3-month, 40 mm in length. Fetal organs already have such systems possessed by an adult. In this age of genital can not distinguish between males and females and looks like a female and heart rate can already be heard.
In the months to 4 measures 56 mm fetus. Head is still dominant over the body, the external genitalia appear different. At week 16 all vital organs are formed. Enlargement of the uterus can already be felt by the mother.
At 5 months into the fetal size 112 mm, while the end of the month to reach 5 size 160 mm fetus. Looks like a human face and hair began to appear throughout the body (lanugo). In the male testes began occupying the place where he will descend into the scrotum. Fetal movement can already be felt by the mother. The lungs are finished formed but not functioning.
In sizes 6 months to have more proportionate body, but seems thin, internal organs are in normal position.
In 7 fetuses appear to thin, wrinkled and red. Developed scrotum and testes began to descend into the scrotum, it was completed in 9 months. nervous system developed enough to regulate the movement of the fetus, if born 10% to survive.
At 8 months into the testis is the scrotum and the body begins to grown fat so it looks smooth and contain. Weight began to rise 70% if born to survive.
At 9 months, the fetus closed more fat (vernix caseosa). Began to appear on the nail tip of fingers and toes.
At month 10, the body of the fetus growing space is reduced and begin to disappear. Lung branching but not fully functional until birth. Parent supplying antibodies and the placenta begin to regression of blood vessels also begin plasenta regression.
Definition and Process of Embryo Formation
The fetus or embryo is a creature which is in the growing in the womb. Gynecology is located in or outside the main body of the parent body (the egg). Growing up is a change from simple forms and the young to form a complex or adult (Wildan orphans, 1990).
Meanwhile, in Microsoft Encarta 2006 stated that the fetus is a vertebrate animal that has not been born at a stage where all the structural characteristics of adults can already known, mainly descendants of people who have not born after eight weeks of growth.
The process of embryo formation :
Spermatogenesis, The transition from going to an active sex cells divide into mature sperm, and involve various kinds of structural changes that take place in sequence. Spermatogenesis took place in the seminiferous tubules and regulated by the hormone and testosterone gonadtotropin (Wildan orphans, 1990).
Phase formation of spermatozoa was divided into three phases:
Sex Cells Primordial
Sex cells of primordial first seen in the embryonic ectoderm of the saccus vitellinus, and a migration to the epithelium germinativum at about 6 weeks to intrauteri life. Each primordial sex cells (oogonia) is surrounded by pregranulosa cells that protect and provide nutrients oogonia and together form a primordial follicle.
Folikel Primordial
A migration of primordial follicles into the ovarian stroma and follicular cortex was produced as many as 200,000. A number of primordial follicles develop during the life of working intrauteri and during childhood, but none reached the cooking. At the time of puberty one follicle can complete the cooking process and called follicle de Graaf, where inside there are sex cells called primary oocytes.
Oosit Primer
Core (nucleus) primary oocytes contain 23 pairs of chromosomes (2n). One pair of chromosomes are chromosomes that determines sex, and called the XX chromosome. Chromosomes called autosomes other. One chromosome consists of two chromatin. Chromatin carry genes called DNA.
Meiosis First division
Meiosis occurs in the ovaries when the follicles de Graaf had finished cooking and before ovulation occurs. Oocyte or ovum nucleus split to separate chromosomes and form two sets that each contain 23 chromosomes. One set of remains larger than the others because it contains all the cytoplasm, the cell is called the secondary oocyte. Smaller cells called the first polar body. Sometimes this primary polar body may divide and will normally degenerate.
This first meiotic division caused haploid chromosomes in oocytes of secondary and primary polar body, also occurs chromatid exchange and the genetic material. Each chromosome is still carrying a chromatid without exchange, but the other one chromatid exchange experience with one chromatid to another chromosome (partner). Thus the two cells contain the same number of chromosomes, but with the genetic material of different patterns.
Oosit Sekunder
The second meiotic division usually occurs only when the head of spermatozoa through the zona pellucida oocyte (ovum). Secondary oocyte divides to form mature ovum and a polar body again, to form two or three polar bodies and a mature ovum, all contain different genetic material. These three polar bodies are normally degenerate. The mature ova that have undergone fertilization began experiencing embryonic development.
Fertilisasi
According to Sri Sudarwati (1990) fertilization is a process of fusion of two kinds of gametes to form a new individual with genetic characteristics derived from both parentalnya. Meanwhile, according Wildan Orphans (1990) fertilization is the entry of spermatozoa into the ovum. After a spermatozoon comes in, the ovum can grow into new individuals.
Spermatozoa around the ovum will produce the enzyme hyaluronidase, an enzyme which breaks protoplasm ova protective order to penetrate an ovum with a little more easily. Enzyme damaging corona radiata and zona pellucida penetration allows for only one sperm only. Body and tail separated from the sperm head immediately after entry into the ovum. Immediately after the two cells together, the two poles of the coil in the core (nucleus) ova having the second meiotic division and are able to unite with the sperm nucleus, chromosome, forming a diploid (2n).
READ MORE - Definition and Process of Embryo Formation
Meanwhile, in Microsoft Encarta 2006 stated that the fetus is a vertebrate animal that has not been born at a stage where all the structural characteristics of adults can already known, mainly descendants of people who have not born after eight weeks of growth.
The process of embryo formation :
Spermatogenesis, The transition from going to an active sex cells divide into mature sperm, and involve various kinds of structural changes that take place in sequence. Spermatogenesis took place in the seminiferous tubules and regulated by the hormone and testosterone gonadtotropin (Wildan orphans, 1990).
Phase formation of spermatozoa was divided into three phases:
- Spermatocytogenesis, Spermatogonia are undergoing mitosis many times that will be the primary spermatocytes. Spermatogonia are primitive structures and can reproduce (divide) by mitosis. Spermatogonia are getting the nutrients from Sertoli cells and develop into primary spermatocytes. Primary spermatocyte chromosomes contain diploid (2n) in the cell nucleus and the experience of meiosis. One spermatocytes will produce two daughter cells, the secondary spermatocytes.
- Stages Meiois, Spermatocytes I (primary) away from the basal lamina, the cytoplasm increased and soon had meiosis I followed by meiosis II.
Sitokenesis in meiosis I and II did not share the complete germ cells separate, but still connected by a bridge sesame (Interceluler bridge). Compared with the spermatocyte I, spermatocyte II has a dark core. - Stages of Spermiogenesis, Is the transformation of spermatids into spermatozoa which includes 4 phases of Golgi phase, cap phase, akrosom phase and maturation phase. The final results of the four mature spermatozoa. Two spermatozoa will carry chromosomes determine the sex of her "X". If any of these spermatozoa unite with the ovum, the pattern of human somatic cells that were 23 pairs of chromosomes will be maintained.
Mature spermatozoon consists of:
- Head (caput), not only contains the core (nucleus) with the chromosome and its genetic material, but also covered by akrosom hyaluronidase-containing enzyme that facilitates the ovum fertilization.
- Neck (servix), connecting the head with the body.
- Body (corpus), responsible for producing the energy needed for motility.
- Tail (cauda), serves to encourage mature spermatozoa into the vas defern and ductus ejakulotorius.
Sex Cells Primordial
Sex cells of primordial first seen in the embryonic ectoderm of the saccus vitellinus, and a migration to the epithelium germinativum at about 6 weeks to intrauteri life. Each primordial sex cells (oogonia) is surrounded by pregranulosa cells that protect and provide nutrients oogonia and together form a primordial follicle.
Folikel Primordial
A migration of primordial follicles into the ovarian stroma and follicular cortex was produced as many as 200,000. A number of primordial follicles develop during the life of working intrauteri and during childhood, but none reached the cooking. At the time of puberty one follicle can complete the cooking process and called follicle de Graaf, where inside there are sex cells called primary oocytes.
Oosit Primer
Core (nucleus) primary oocytes contain 23 pairs of chromosomes (2n). One pair of chromosomes are chromosomes that determines sex, and called the XX chromosome. Chromosomes called autosomes other. One chromosome consists of two chromatin. Chromatin carry genes called DNA.
Meiosis First division
Meiosis occurs in the ovaries when the follicles de Graaf had finished cooking and before ovulation occurs. Oocyte or ovum nucleus split to separate chromosomes and form two sets that each contain 23 chromosomes. One set of remains larger than the others because it contains all the cytoplasm, the cell is called the secondary oocyte. Smaller cells called the first polar body. Sometimes this primary polar body may divide and will normally degenerate.
This first meiotic division caused haploid chromosomes in oocytes of secondary and primary polar body, also occurs chromatid exchange and the genetic material. Each chromosome is still carrying a chromatid without exchange, but the other one chromatid exchange experience with one chromatid to another chromosome (partner). Thus the two cells contain the same number of chromosomes, but with the genetic material of different patterns.
Oosit Sekunder
The second meiotic division usually occurs only when the head of spermatozoa through the zona pellucida oocyte (ovum). Secondary oocyte divides to form mature ovum and a polar body again, to form two or three polar bodies and a mature ovum, all contain different genetic material. These three polar bodies are normally degenerate. The mature ova that have undergone fertilization began experiencing embryonic development.
Fertilisasi
According to Sri Sudarwati (1990) fertilization is a process of fusion of two kinds of gametes to form a new individual with genetic characteristics derived from both parentalnya. Meanwhile, according Wildan Orphans (1990) fertilization is the entry of spermatozoa into the ovum. After a spermatozoon comes in, the ovum can grow into new individuals.
Spermatozoa around the ovum will produce the enzyme hyaluronidase, an enzyme which breaks protoplasm ova protective order to penetrate an ovum with a little more easily. Enzyme damaging corona radiata and zona pellucida penetration allows for only one sperm only. Body and tail separated from the sperm head immediately after entry into the ovum. Immediately after the two cells together, the two poles of the coil in the core (nucleus) ova having the second meiotic division and are able to unite with the sperm nucleus, chromosome, forming a diploid (2n).
Thursday, October 15, 2009
Bleeding ANTEPARTUM

Bleeding ANTEPARTUM
Antepartum hemorrhage is bleeding in the street were born after 20 weeks of pregnancy. (1)
Classification of antepartum haemorrhage
1. Placenta previa
2. Solusio placenta
3. Antepartum bleeding source unknown (idiopathic)
The characteristics of placenta previa: (2)
1. Bleeding without pain
2. Recurrent bleeding
3. Fantastic fresh red bleeding
4. The presence of anemia and in accordance with Schok bleeding
5. Slow emergence
6. The timing of when pregnant
7. His usually no
8. Flavor not tense (regular) during palpation
9. Fetal heart rate was
10. Placental tissue palpable in the vagina in check
11. Decrease in the head does not enter the door above the pelvis
12. Presentations may be abnormal.
Solusio characteristics of the placenta: (2)
1. Bleeding with pain
2. Bleeding does not repeat
3. Red-brown color bleeding
4. The presence of anemia and Schok inconsistent with bleeding
5. Sudden emergence
6. The timing of when pregnant inpartu
7. His is
8. Sense of anticipation as palpation
9. Fetal heart rate usually does not have
10. Amniotic palpable tension in check in the vagina
11. The decrease can head into the door of the pelvis
12. Not related to presentation
Placenta Previa
_______________
Placenta previa is an abnormal placenta that is situated on the lower uterine segment that covers part or all of the opening of the birth canal (os uteri internum). (2)
Classification of placenta previa based terabanya placental tissue through the opening of the birth at a particular time: (2)
1. Placenta previa totalis: if the opening of roads covered by the placenta is born.
2. Lateral placenta previa: if only partially covered the opening of the birth canal
by the placenta.
3. Placenta previa marginalis: if the edge of the placenta was right on the edge of the
opening of the birth canal.
4. Placenta previa low position: if the placenta is 3-4 cm above the edge
opening of the birth canal.
Aetiology of placenta previa is not clear. (2)
Diagnosis of placenta previa: (2)
1. Anamnesis: the existence of vaginal bleeding in pregnancy over 20 weeks
and lasted for no reason.
2. External examination: frequently found abnormalities location. If the location of the head of the
head does not enter the door of the pelvis.
3. Inspekulo: the blood of the os uteri eksternum.
4. Ultrasound to determine the location of the placenta.
5. Determining the location of the placenta directly with the touch directly via
examination of the cervical canal but this is very dangerous because it can
cause bleeding a lot. Therefore this method is only done
above the operating table.
Management of placenta previa: (2)
1. Conservative if:
a. Less than 37 weeks of pregnancy.
b. Bleeding does not exist or is not much (Hb still in the normal range).
c. Patient residence near the hospital (can take
travel for 15 minutes).
2. Handling active when:
a. Bleeding a lot of pregnancy regardless of age.
b. Age pregnancy 37 weeks or more.
c. Child dies
Conservative treatment in the form:
- Rest.
- Provide hematinik and spasmolitik unntuk overcome anemia.
- Give antibiotics if there indikasii.
- Ultrasound, hemoglobin, and hematocrit.
If for 3 days did not bleed after conservative treatment then do a gradual mobilization. Patients discharged if still no bleeding. If bleeding occur immediately brought to the hospital and should not perform intercourse.
Active handling of:
- Labor per vaginal.
- Labor per abdominal.
The patient is prepared for examination on the operating table (double set-up) that is in a state ready for operation. If the examination obtained:
1. Placenta previa marginalis
2. Placenta previa low position
3. Lateral Marginal placenta or fetal death and in which the cervix is ripe,
head had entered the door of the pelvis and there was no bleeding or only
then do a little bleeding amniotomi followed by oxytocin drips
on partus per vaginal if fail drips (in accordance with the termination protap
pregnancy). If there is bleeding a lot, do seksio fault.
Indications do seksio fault:
- Placenta previa totalis
- Bleeding a lot without stopping.
- Percentage abnormal.
- Narrow pelvis.
- State of the cervix is not favorable (beelum mature).
- Emergency fetus
In circumstances where possible do not fault the seksio do Willet installation pliers or Braxton Hicks version.
Solusio Placenta
________________
Separation of the placenta is Solusio some or all of the normal implantation of the placenta on the fetus before birth. (2)
Solusio classification based on clinical signs of the placenta and the degree of release of the placenta, namely:
1. Light: Bleeding less 100-200 cc, the uterus is not tense, there is no sign of
renjatan (Schok ), fetal life, the release of the placenta is less 1 / 6 of the surface, the levels
more plasma fibrinogen 120 mg%.
2. Medium: 200 cc more bleeding, uterine tension, there is a sign of pre renjatan,
severe fetal or fetus has died, the release of the placenta 1/4-2/3
surface, plasma fibrinogen levels of 120-150 mg%.
3. Weight: Uterus tetanik tense and contract, there are signs renjatan, fetal
death, the release of the placenta may occur over 2 / 3 part or whole.
Etiology unclear solusio placenta. (2)
Management of placenta solusio: (2)
Depending on the severity of the case. In light of the placenta is solusio break, giving sedatives and then determine whether the symptoms of the more progressive or it will stop. When the process stops gradually, the patient mobilized. During examination treatment Hb, fibrinogen, hematocrit and platelets.
In solusio placenta and the weight it was intended to overcome the handling renjatan, improving anemia, stop bleeding and to empty the uterus as quickly as possible. Rx include:
1. Provision of blood transfusion
2. Solving membranes (amniotomi)
3. Oxytocin infusion
4. If necessary seksio fault.
If the diagnosis is clinically placenta solusio already be enforced, there is minimal bleeding which 1000 cc of blood transfusion should be given a minimum of 1000 cc. Amniotic solved soon in order to reduce the strain of the uterine wall and to accelerate the delivery of oxytocin infusion was given 5 UI dekstrose in 500 cc 5%.
Fault Seksio done when:
1. Labor is not completed or not expected to be completed in 6 hours.
2. Bleeding a lot.
3. No opening of 4 cm or less.
4. Narrow pelvis.
5. Location of latitude.
6. Severe pre eclampsia.
7. Pelvic score less than 5.

Vasa Previa
Vasa previa is a condition in which the fetal umbilical blood vessels are inserted with the vilamentosa ie membranes. (2)Etiology unclear vasa previa. (2)
Diagnosis of vasa previa: (2)
On examination of the vagina on palpable vascular membranes. Screening also can be done with inspekulo or amnioskopi. When you are bleeding it will be followed by fetal heart rate irregular, deceleration or bradikardi, especially when perdahan occurs when or shortly after the membranes rupture. This blood comes from the fetus and to know it can be done with the test Apt and Kleihauer-Betke tests and peripheral blood removal.
Management of vasa previa: (2)
Highly dependent on the status of the fetus. If there is doubt about the viability of the fetus, determine the age of first pregnancy, fetal size, lung maturity and fetal well-being monitoring by ultrasound and kardiotokografi. If the fetus is mature enough to live and can be done immediately seksio fault but if the fetus is dead or immature, performed vaginal delivery.
HELLP SYNDROME
HELLP syndrome is a pre eclampsia and eclampsia are accompanied by the hemolysis, increased liver enzymes, liver dysfunction and thrombocytopenia. (H = haemolysis; EL = Elevated Liver Enzymes; LP = low platelets count)
The diagnosis of HELLP syndrome:
1. Signs and symptoms are not typical: nausea, vomiting, headache, malaise,
weaknesses. (All signs and symptoms similar to viral infection).
2. Signs and symptoms of pre eclampsia: hypertension, proteinuria, epigastric pain,
edema, and increased uric acid.
3. The signs of hemolysis intravaskuler:
a. The increase in LDH, AST and bilirubin indirect.
b. Decrease in haptoglobin.
c. Peripheral blood swabs: the fragmentation of erythrocytes.
d. Increased urobilinogen in the urine.
4. Signs of damage / dysfunction hepatosit cells: Increase in ALT, AST, LDH.
5. Thrombocytopenia: Platelets 150.000/ml or less.
All pregnant women with complaints of pain in the quadrant of the abdomen without regard to presence or absence of signs and symptoms of pre eclampsia HELLP syndrome should be considered.
HELLP syndrome classification:
1. Classification Mississippi
Class I: Platelets 50.000/ml or less; serum LDH 600,000 IU / l or more;
AST and / or ALT 40 IU / l or more.
Class II: Platelets over 50,000 to 100.000/ml; serum LDH 600,000 IU / l
or more; AST and / or ALT 40 IU / l or more.
Class III: Platelets over 100,000 to 150.000/ml; serum LDH 600,000 IU / l
or more; AST and / or ALT 40 IU / l or more.
2. Classification Tennessee
Complete class: Platelets less 100.000/ml; 600,000 LDH IU / l or more;
AST 70 IU / l or more.
Class is incomplete: If found 1 or 2 of the signs above.
Diagnosis versus pre-eclampsia HELLP syndrome:
1. Trombotik angiopati
2. Fibrinogen consumptive disorders, such as:
- Acute fatty liver of pregnancy.
- Hypovolaemia heavy / heavy bleeding.
- Sepsis.
3. Connective tissue disorders: SLE.
4. Primary renal disease.
Medical Therapy:
1. Following medical therapy: pre eclampsia and eclampsia.
2. Laboratory for examination and LDH platelets every 12 hours.
3. When platelets less 50.000/ml or any sign of the consumptive coagulopathy
should be checked:
- Left protombin
- Partial thromboplastin time
- Fibrinogen.
4. Giving dexamethasone rescue:
a. Antepartum: double strength given dexamethasone (double dose). If
obtained:
- Platelets less 100.000/cc or
- Platelets 100.000-150.000/cc and with eclampsia, severe hypertension, pain
epigastrium, symptoms of fulminant then given dexamethasone 10 mg IV
every 12 hours.
b. Postpartum: Dexamehasone given 10 mg intravenously every 12 hours 2 times
then followed by 5 mg intravenously every 12 hours 2 times.
c. Dexamethasone therapy was stopped if there is:
1. Improvements laboratory: Platelets more 100.000/ml and decreased LDH.
2. Repair clinic signs and symptoms of pre eclampsia - eclampsia.
5. Can be considered providing:
a. Platelet transfusions when platelets less 50.000/cc.
b. Antioxidants.
Attitude: The management of obstetric
Attitudes toward pregnancy in HELLP syndrome, which is active the pregnancy terminated (termination) without regard to age pregnancy. Vaginal delivery can be done or perabdomen.
Pre eclampsia LIGHTER
Mild pre eclampsia is a pregnancy specific syndrome with decreased perfusion to the organs due to activation vasospasme and endothel.
Diagnostic criteria mild pre eclampsia:
1. Blood Pressure 140/90 - 160/110 mmHg; increase in systolic blood 30 mmHg or
more and an increase in diastolic blood 15 mmHg or more, not included
in the diagnostic criteria for pre eclampsia but need careful observation.
2. Proteinuria 300 mg/24 hours or more the amount of urine or dipstick +1 or more.
3. Edema: local in the legs were not included in the diagnostic criteria except
anasarka.
Management of mild pre eclampsia can be:
1. Outpatient (ambulatoir)
2. Inpatient (hospitalisasi)
Management of outpatient (ambulatoir):
1. No absolute must tirah lie, recommended ambulasi wanted. In
Indonesia tirah lying still needed.
2. Regular diet: do not need a special diet.
3. Pre natal vitamins.
4. No need to salt intake restriction.
5. There is no need granting diuretic, antihypertensive and sedativum.
6. Visits to the hospital every week.
Management of inpatient care (hospitalisasi):
1. Indications of mild pre eclampsia hospitalized (hospitalisasi)
a. Hypertension that persist for over 2 weeks.
b. Proteinuria in a settlement for over 2 weeks.
c. The results of abnormal laboratory tests.
d. The presence of symptoms or signs 1 or more severe pre eclampsia.
2. Inspection and monitoring of the mother
a. Measurement of blood pressure every 4 hours unless you sleep.
b. A careful observation of edema in the face and abdomen.
c. Weighing heavily on the mother's body in the hospital and
weighing done every day.
d. Observation with symptoms of pre eclampsia closely with the impending
eclampsia:
- Pain or occipital frontal head.
- Disturbance visus
- Upper right quadrant pain stomach
- Epigastric pain
3. The laboratory
a. Dipstick proteinuria at the time of entry and followed at least 2 days later.
b. Hematocrit and platelet 2 times a week.
c. Liver function tests 2 times a week.
d. Kidney function tests with measurement of serum creatinine, uric acid and BUN.
e. Measurement of the production of urine every 3 hours (not necessarily with the catheter fixed).
4. Fetal welfare checks
a. Observations fetal movements every day
b. NST 2 times a week
c. Fetal biophysical profile, if the non-reactive NST.
d. Evaluation of fetal growth with ultrasound every 3-4 weeks.
e. Umbilical artery Doppler ultrasound, uterine artery.
Medical treatment:
1. Basically the same as ambulatoar therapy.
2. If there is improvement of symptoms and signs of pre eclampsia and age
pregnancy 37 weeks or more, you still need to be observed for 2-3 days
then be discharged.
Management of obstetric
Depending on the age of pregnancy:
a. If the patient does not inpartu
- Age less than 37 weeks of pregnancy
If signs and symptoms did not worsen, pregnancy can be maintained until
term.
- Age 37 weeks of pregnancy or more
1. Maintained pregnancy until the onset partus arise.
2. If the cervix is ripe on the estimated date of delivery can be considered
performed labor induction.
b. If the patient has inpartu
The journey can be followed by delivery Friedman graphics or partograf WHO.
During hospitalization conducted consultations on:
1. Part of eye disease
2. Part of heart disease
3. Other parts of indications.
Bleeding IN PREGNANCY YOUNG
Bleeding in pregnancy is vaginal bleeding in pregnancy is less than 22 weeks.
General handling young bleeding in pregnancy:
- Make a quick assessment of the general state mengenaii patients, including
vital signs (pulse, blood pressure, respiration, and temperature).
- Check for signs of shock (pale, berkerringat many, fainting, systolic pressure
less than 90 mm Hg, pulse over 112 beats per minute).
- If suspected happens shock, shock treatment mullai soon. If no visible signs of
signs of shock, still consider this possibility when helpers do
evaluation of the condition of women because the condition may worsen with
fast. In the event of shock, it is important to start treatment of shock with
soon.
- If the patient is in a state of shock, the possibility of ectopic pregnancy pikirkaan
upset.
- Install an IV infusion with a large ((16 G or more), given saline solution
physiological or Ringer's lactate with a rapid drop (500 cc in the first 2 hours).
Diagnosis of bleeding in pregnancy:
1. Think about the possibility of ectopic pregnancy in women with anemia, a disease
pelvic inflammation (pelvic inflammatory disease-PID), symptoms or complaints abortion
unusual pain.
Note: If suspected ectopic pregnancy, do the inspection
bimanual carefully for early ectopic pregnancy can be reached easily
rupture.
2. Think about the possibility of abortion in women of reproductive age who have
missed a period (over 1 month since the last menstruation) and have 1 or more
the following signs: bleeding, rigid abdomen, spending some product of conception,
a dilated cervix or uterus that is smaller than it should.
3. If abortion is a possible diagnosis, identify and quickly handle
there are complications.
1. Diagnosis abortion imminens:
- Spots of bleeding until bleeding is. Mild bleeding
It took about 5 minutes to wet gauze or cloth
clear.
- The cervix is closed.
- Uterus in accordance with gestational age.
- Symptoms / signs: lower abdominal cramps and uterine software.
2. The diagnosis of disturbed ectopic pregnancy:
- Spots of bleeding until bleeding is.
- The cervix is closed.
- Uterus slightly larger than the normal gestation
- Symptoms / signs: unsteady or faint, lower abdominal pain, pain porsio rocking,
adneksa mass, and intra-abdominal free fluid.
3. The diagnosis of complete abortion:
- Spots of bleeding until bleeding is.
- The cervix is closed or open.
- The uterus is smaller than the normal gestation
- Symptoms / signs: little or no lower abdominal pain, and history ekspulsi results
conception.
4. Diagnosis abortion insipiens:
- The bleeding was so massive (many). Heavy bleeding requires
less 5 minutes to wet gauze or clean cloth.
- The cervix is open.
- Uterus with age pregnancy.
- Symptoms / signs: cramping / lower abdominal pain, and has not happened ekspulsi results
conception.
5. Diagnosis abortion inkomplit:
- The bleeding was so massive (many).
- The cervix is open.
- Uterus with age pregnancy.
- Symptoms / signs: cramping / lower abdominal pain, and some of the results ekspulsi conception.
6. Molar abortion diagnosis:
- The bleeding was so massive (many).
- The cervix is open.
- Uterus soft and larger than the age of pregnancy
- Symptoms / signs: nausea / vomiting, abdominal cramps down, syndrome-like pre
eclampsia, there is no fetus, and out of networks like wine.
Signs and symptoms include abortion under the abdominal pain, pain free, the uterus felt weak, continue bleeding, weakness, lethargy, fever, smelly vaginal secretions, secretions & pus from the cervix, and cervical pain rocking. Complications were infection / sepsis. Handling is starting to give antibiotics as soon as possible before doing the manual vacuum aspiration. Of antibiotic ampicillin 2 g IV every 6 hours plus gentamicin 5 mg / kgbb IV every 24 hours plus metronidazole 500 mg IV every 8 hours until the mother's fever-free 48 hours.
Other signs and symptoms are pain / stiff in the abdomen, pain free, abdominal distension, abdominal feel tight & hard, shoulder pain, nausea, vomiting, and fever. Complication is injury of the uterus, vagina or bowel. Handling is done laparotomy to repair injury and do manual vacuum aspiration, respectively. Ask for further assistance if needed.
Types of Abortion
The types of abortion:
1. Spontaneous abortion
2. Deliberate abortion
3. Unsafe abortion
4. Septic abortion
Spontaneous abortion is the termination of pregnancy before the fetus reaches viability (22 weeks of gestation). Stages of spontaneous abortion include:
1. Imminens abortion (pregnancy may continue).
2. Insipiens abortion (the pregnancy will not continue and will grow to
inkomplit abortion or abortion complete).
3. Inkomplit abortion (some of the conceptus has been issued).
4. Complete abortion (all the conceptus has been issued).
Deliberate abortion is a process of termination of pregnancy before the fetus reaches viability.
Unsafe abortion is a procedure performed by someone who is inexperienced, or in environments that do not meet minimal medical standards or both.
Septic abortion is that abortion complications of infection, sepsis can be derived from organisms causing infection if the rise of lower urinary tract after a spontaneous abortion or abortion is not safe. Sepsis is likely to occur if there is a remainder of conception or delays in spending the conceptus. Sepsis is a common complication of unsafe abortion by using the equipment.
Handling
If you suspect an unsafe abortion occurs, check for signs of infection or injury of the uterus, vagina and intestinal, vaginal irrigation done to remove vegetation, the local drugs or other substances.
Handling abortion imminens:
1. Do not need special treatment or a total lie tirah.
2. Do not do excessive physical activity or sexual intercourse.
3. If the bleeding:
- Stop: do ante-natal care as usual, do the assessment if
bleeding occurs again.
- Keep going: the value of fetal condition (pregnancy test or ultrasound). Do
confirm the possibility of other causes. The bleeding continues,
especially if the uterus is found larger than expected,
may indicate multiple or molar pregnancy.
4. No need hormonal therapy (estrogen or progestin) or tokolitik (eg
Salbutamol or indomethacin) because these drugs can not prevent
abortion.
Handling abortion insipiens:
1. If age less than 16 weeks of pregnancy, do an evaluation of the uterus by aspiration
manual vacuum. If the evaluation can not, do immediately:
- Give ergometrin 0.2 mg intramuscular (can be repeated after 15 minutes when
necessary) or 400 mcg of misoprostol orally (may be repeated after 4 hours if
necessary).
- Immediately make preparations for spending the conceptus from the uterus.
2. If age over 16 weeks of pregnancy:
- Wait ekspulsi spontaneous conception and evaluation of the remnants of conception.
- If necessary, take 20 units of oxytocin infusion in 500 ml of intravenous fluids
(physiological salt solution or Ringer's lactate) at 40 drops per
minutes to help ekspulsi the conceptus.
3. Be sure to keep monitoring the condition of women after treatment.
Handling abortion inkomplit:
1. If the bleeding is not how much, and less 16 weeks of pregnancy,
evaluation can be done digitally or with pliers ova for
out the conceptus is out through the cervix. If bleeding
stopped, give 0.2 mg of intramuscular ergometrin or 400 mcg misoprostol per
oral.
2. If bleeding a lot or continue and gestational age less than 16
weeks, the rest of the conceptus evaluation with:
- Manual vacuum aspiration is the chosen method of evaluation. Evacuation
with a sharp curette should only be done if the manual vacuum aspiration
not available.
- If evacuation can not be done immediately, give 0.2 mg ergometrin
intramuscular (repeated after 15 minutes if necessary) or 400 mcg misoprostol
per oral (may be repeated after 4 hours if necessary).
3. If pregnancy over 16 weeks:
- Give 20 units of oxytocin infusion in 500 ml of intravenous fluids (physiological salt
or Ringer's lactate) at 40 drops per minute until there is
ekspulsi the conceptus.
- If you need to give misoprostol 200 mcg per vaginal every 4 hours until
occurs ekspulsi the conceptus (maximum 800 mcg).
- Evaluate the rest of the conceptus is left in the uterus.
4. Be sure to keep monitoring the condition of women after treatment.
Handling of complete abortion:
1. No need to evaluate again.
2. Observations to see a lot of bleeding.
3. Be sure to keep monitoring the condition of women after treatment.
4. If there is anemia, sulfas ferrosus tablets provide 600 mg per day
for 2 weeks. If severe anemia, blood transfusions given.
5. Post-abortion care counseling and monitoring information.
Monitoring Post-Abortion
__________________________
Incidence of spontaneous abortion approximately 15% (1 of 7 pregnancies) of all pregnancies.
The requirements begin contraceptive methods within 7 days of an unwanted pregnancy:
1. There were no severe complications that require further treatment.
2. Mothers receive counseling and assistance in choosing a method sufficiently
most appropriate contraception.
Post-abortion contraceptive methods:
1. Condoms
- When the application immediately.
- Effectiveness depends on the level of client discipline.
- Can prevent sexually transmitted diseases.
2. Contraceptive pill
- When the application immediately.
- Self-effective but needs obedience clients to take a pill regularly.
3. Injections
- When the application immediately.
- Counseling for the choice of single or combination of hormones.
4. Implant
- When the application immediately.
- If the couple had 1 child or more and wanted to contraception
long-term.
5. Intrauterine device
- When the application immediately and after the patient recovered.
- Postpone the insert if hemoglobin less than 7 g / dl (anemia) or if the suspected
infection.
6. Tubectomy
- When the application immediately.
- For couples who want to stop fertility.
- If you suspect an infection, delay the procedure until the situation clearly. If
hemoglobin less than 7 g / dL, delay until the anemia has improved.
- Provide an alternative method (such as condoms).
Some women may require:
1. If the client never immunized, give a booster tetanus toxoid 0.5 ml or if
wall of the vagina or cervical canal was contaminated wounds.
2. If the immunization history is not clear, given anti-tetanus serum 1500 units
intramuscular followed by 0.5 ml of tetanus toxoid after 4 weeks.
3. Treatment for sexually transmitted diseases.
4. Cervical cancer screening.
Pregnancy Ektopik Bothered
___________________________
Ectopic pregnancy is a pregnancy with implantation occurs outside the uterine cavity. Fallopian tube is the most common place of implantation of ectopic pregnancy (over 90%).
Signs and symptoms of ectopic pregnancy vary greatly depending on whether the pregnancy broke. Important tool that can be used to diagnose ectopic pregnancies that rupture is of the serum pregnancy test combined with an ultrasound examination. If you obtained the day! Not frozen blood begin treatment.
Signs and symptoms of ectopic pregnancy:
1. Symptoms of early pregnancy in the form of spots or irregular bleeding, nausea, enlarged
breast, discoloration of the vagina & cervix, cervical perlunakan,
enlargement of the uterus, frequency of urination increases.
2. Pain in the abdomen and pelvis.
Signs and symptoms of disturbed ectopic pregnancy:
1. Collapse and fatigue.
2. Pulse rapid and weak (110 times per minute or more).
3. Hypotension.
4. Hypovolemia.
5. Acute abdominal and pelvic pain.
6. Abdominal distension. Abdominal distension with shifting dullness is
evidence of free blood.
7. Pain free.
8. Pale.
Differential diagnosis of ectopic pregnancy is linked imminens abortion. Another appeal diagnosis is pelvic inflammatory disease acute & chronic, ovarian cysts (twist or rupture) and acute Appendisitis. Ultrasound can distinguish between an ectopic pregnancy, abortion and imminens twisted ovarian cyst.
Initial handling of ectopic pregnancy:
1. Immediately do blood tests and laparatomi cross. Do not wait for the blood
before performing surgery.
2. If there are no facilities, immediately refer to the more complete facilities and do
initial assessment.
3. In laparatomi, exploring both ovaries and fallopian tubes:
- Severe tubal damage: do salpingektomi (the conceptus and the tuba
both released). This is the treatment of choice in most
case.
- Damage to the small tube: do salpingostomi (the conceptus issued
and fallopian maintained). This is done by considering
conservation of fertility because of the risk of subsequent ectopic pregnancy is high.
If there is bleeding a lot can be done autotransfusi if intraabdominal blood still fresh and not infected or contaminated (by the end of pregnancy, the blood can be contaminated with amniotic fluid and others that should not be used for autotransfusi). Blood can be collected before surgery or after abdominal opening:
1. As the mother lay on the operating table before surgery and abdominal
looked tense due to the blood gathering, as it allows for
insert the needle through the abdominal wall and the blood collected is set
donors.
2. Alternatively, open the abdomen:
- Take the blood into a place and using the blood filter
screen to separate the blood clot.
- Clean the top of the blood bag with an antiseptic and open
with a sterile knife.
- Pour the blood of these women into the bag and re-enter
through a set of filters in the normal way.
- If there is no donor bag with anticoagulant, add sodium
citrate 10 ml for every 90 ml of blood.
Further handling:
1. Before allowing the mother came home, doing counseling and advice on
fertility prognosis. Given the increased risk of ectopic pregnancy
next, counseling and provision of contraceptive methods contraceptive methods,
if desired, is essential.
2. Fix sulfas anemia with ferrous 600 mg / hr per orally for 2 weeks.
3. Schedule the next visit to monitoring within 4 weeks.
Hydatidiform mole
_______________
Molar pregnancy is an abnormal proliferation of the villi khorialis.
Initial handling of molar pregnancy:
If the diagnosis of molar pregnancy has been established, evaluate the uterus:
- If required dilatation of the cervix, gunakkan block paraservikal.
- Discharging with manuaal vacuum aspiration is safer than kuretase
sharp. Risk of perforation by using a sharp curette is high enough.
- If the source is a vacuum tube manual, prepare a vacuum aspiration equipment
manual at least 3 sets to be used interchangeably to
uteri finished pouch emptying. The contents of the uterus, but significant enough to
quickly emptied.
Subsequent handling of molar pregnancy:
- Patients are encouraged to use hormonal konntrasepsi (if still want to
children) or tubectomy if you want to stop fertility.
- Conduct monitoring every 8 weeks selaama least 1 year post-evacuation
by using a urine pregnancy test because of the risk
trophoblast disease persist or khoriokarsinoma. If test
urine pregnancy with no negative after 8 weeks or becomes positive
back in the first 2 years, refer to a tertiary medical center for
monitoring and further treatment.
Abnormalities in the Fetus
 Abnormalities in the fetus
Abnormalities in the fetusDown syndrome is the excess number of strands in the chromosome 21 so that children grow up with mental retardation, heart defects, hearing and poor vision, muscle weakness and trends of cancer of white blood cells (leukemia).
Other disorders that can be detected since the fetus is Patau syndrome, which causes severe interference in the development of the brain, heart, kidneys, lips and oral cavity. If severe symptoms, the baby may die a few hours or several weeks after birth. Edward Yang's syndrome also cause mental retardation, growth disturbance, head size and small hips and hands and feet abnormalities. Detection of abnormalities after birth such as phenylketonuria and congenital hypothyroidism was also performed. Phenylketonuria is a metabolic disorder of amino acid phenylalanine-forming protein that causes the growth barriers and mental retardation. Given the early, abnormalities can be prevented by minimizing the intake of phenylalanine there is lots of meat, eggs, fish, milk, cheese, and administration of drugs or certain vitamins. Congenital hypothyroidism is a result of disease or lack of thyroid hormone is not produced. Since the thyroid is a growth hormone, patients will experience a physical growth of mental disorders. Prevention with thyroid hormone supplements as early as possible.
The exact cause of preeclampsia and eklamsia not known until now but high levels of homocysteine in the blood can increase the risk of eklamsi 3. One way to reduce homocysteine levels in the blood is an adequate diet is the consumption of folic acid, vitamin B6, B12. With increasing blood levels of folate in the homocysteine level will be lowered so that the expected risk can preklamsi and reduced eklamsi. While homocysteine itself is an amino acid found in blood. Several studies have shown that the amount of homocysteine in the blood affects the disease associated with blood vessels such as stroke, blood vessel disorder and coronary heart disease. In pregnant women, high levels of homocysteine will result in pregnancy poisoning disease called eklamsia and preklamsia. The high levels of homocysteine in the blood triggered by diet and genetic factors. A diet containing folate and other B vitamins will help to reduce levels of homocysteine in the blood, so the risk of disease can preklamsi and eklamsia reduced.
Subscribe to:
Posts (Atom)